Taking care of patient self-care
 With minor ailments taking up nearly a fifth of GP workload, Chris Chapman looks at why patients are still turning up at surgeries and not community pharmacies
With minor ailments taking up nearly a fifth of GP workload, Chris Chapman looks at why patients are still turning up at surgeries and not community pharmacies
Getting patients to treat self-limiting conditions themselves is vital for the future of the NHS. Minor ailments take up a fifth of GP workload, responsible for 57 million consultations. Developing a culture of self-treatment is the only way the NHS will be able to curtail its spending and ease the demands of a system already creaking under the strain.
Last Wednesday, experts from across the NHS gathered at a self-care symposium organised by the PAGB and Royal College of General Practitioners to flesh out a game plan on how this could be delivered. The consensus was that community pharmacy had a central role – but there were barriers that need to be overcome.
The first is getting patients to recognise pharmacy’s skill set. “It’s important to big up the role of pharmacy, to give patients the confidence to treat their conditions,” says Jeremy Taylor, chief executive of patient charity National Voices.
“Men hugely under-use pharmacy,” adds Peter Baker, chief executive of the Men’s Health Forum. “They are not aware pharmacies can dispense advice as well as tablets, are open long hours, and don’t require an appointment. Pharmacies are not marketing themselves enough to men.”
But this isn’t a new idea: despite pilots from the Department of Health aiming to boost patient awareness of what pharmacy can provide locally, warnings of the sector’s lack of publicity sound like a broken record. And the figures speak for themselves.
According to a PAGB survey of 3,052 minor ailments, only 12-15 per cent of patients, depending on social grade, asked a pharmacist for advice. Between 15 and 24 per cent consulted their GP or practice nurse.
However, BMA GP committee chair Dr Laurence Buckman says it’s not just patients who need to change their attitudes.
“We’ve got to get patients to see pharmacy as a source of information,” he says, “and that requires pharmacists to feel that way too. Most do, and are proud of their professional role… but pharmacists have to feel confident to say ‘if you’re no better, come back’. The person who deals with it first should be the first response.”
Perhaps some criticism is justified. Pharmacists, like all health professionals, have a little voice in the back of their mind during every consultation, asking ‘what if…?’.
A child’s rash is highly unlikely to be an indicator for meningitis, but many pharmacists would feel uncomfortable in ruling it out. Telling patients to go to see their GP if symptoms don’t improve is a safety net, if not sometimes the only sensible option available.
But this notion of pharmacy shows a lack of understanding from medical colleagues on what pharmacists provide. According to the PAGB survey, while 12-15 per cent of patients said they consulted a pharmacist, only around 2 per cent said they were referred on to a GP. Pharmacists are taking responsibility for treatment. And as PAGB director of health policy Gopa Mitra points out: “Pharmacists… are already [giving advice]. They’ve been doing this for decades… their normal role is advice.”
The problem, says Ms Mitra, is that while pharmacists are capable and confident of giving advice, they are not going far enough.
“Around £700 million OTC medicines are sold each year in the UK,” she says. “That’s 700 million opportunities to give advice. And that’s something we haven’t made enough of.”
And according to Ms Mitra, community pharmacists can’t wait for a publicity campaign to deliver results. “It needs to come from the profession itself,” she argues. “It’s suggesting a fundamental role change… we need to say that self-care is the norm.”
Ms Mitra has a point. Ultimately, pharmacists have it within their power to transform self-care into the status quo. When pharmacists are available to offer advice on how to self-medicate, word of mouth quickly takes hold, creating informed patients.
This in turn changes patient attitudes toward self-care, easing the burden on the NHS. And while GPs may lack understanding of what pharmacists do, the strongest change in viewpoint will only occur when surgery waiting rooms empty thanks to the care pharmacists deliver.
Self-care has to be a priority for change in the NHS, and it’s a new way of thinking that needs pharmacy at the vanguard.
[SOURCE]








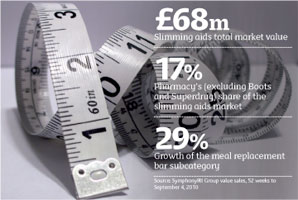
 Subcategories should be organised so customers can distinguish between meal replacements and weight loss aids, while P treatments such as Alli should be clearly signposted behind the counter, adds Boots pharmacist Angela Chalmers.
Subcategories should be organised so customers can distinguish between meal replacements and weight loss aids, while P treatments such as Alli should be clearly signposted behind the counter, adds Boots pharmacist Angela Chalmers.






 Where they work, this should all bode well for pharmacy. And the good news is that C+D has found, using the Freedom of Information Act, that in the last 18 months 96 per cent of trusts have met with their LPCs to discuss the PNA (see p6), which must be a start at least. But multiples have told C+D the PNAs they have seen are not consistent, with some good and others “a mish-mash mosaic”
Where they work, this should all bode well for pharmacy. And the good news is that C+D has found, using the Freedom of Information Act, that in the last 18 months 96 per cent of trusts have met with their LPCs to discuss the PNA (see p6), which must be a start at least. But multiples have told C+D the PNAs they have seen are not consistent, with some good and others “a mish-mash mosaic” 
 Ms Gordon said a meaningful outcomes base was needed, and her view was echoed by director of pharmacy at Lloydspharmacy Andy Murdock (pictured). Mr Murdock invited anyone to let him know about pharmacy interventions that had meaningful outcome measures, warning: “The outcome-based framework will be very hard to measure. We only have measurements for asthma and COPD.”
Ms Gordon said a meaningful outcomes base was needed, and her view was echoed by director of pharmacy at Lloydspharmacy Andy Murdock (pictured). Mr Murdock invited anyone to let him know about pharmacy interventions that had meaningful outcome measures, warning: “The outcome-based framework will be very hard to measure. We only have measurements for asthma and COPD.”